TRAVEL MEDICAL INSURANCE PLAN
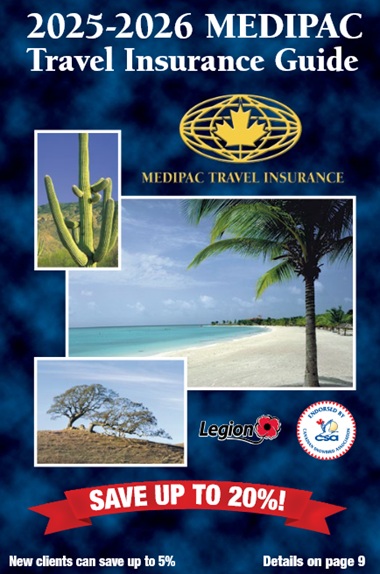
Travel Insurance Guide
- Program & insurance benefits
- Copy of travel insurance policy
- Coverage options available
- Tips on how to save
- Unique discounts – NEW clients too
- Rate categories and premiums
Download
Travel Insurance Plan
Travel Emergency Medical Insurance Policy
- Benefits
- Definitions
- Eligibility requirements
- What you should do in an emergency
- General Limitations and Exclusions
- How to present a claim
- Refund policy
Download
Travel Insurance Plan
Canadian Travel Health Insurance Application
- Medical questions
- Determine eligibility and rate category
- Insurance contract declaration
- Payment options
Download
Travel Insurance Plan

Emergency Contact Guide
- When would I be contacted?
- When to contact Medipac
- Responsibilities as the Emergency Contact
- Policy and contact information
Download
Travel Insurance Plan
TRAVEL INSURANCE OPTIONS
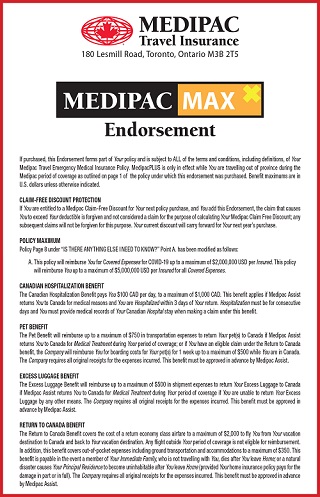
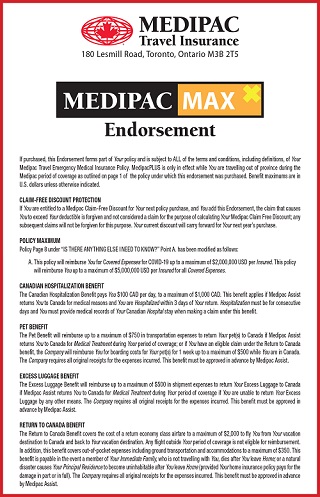
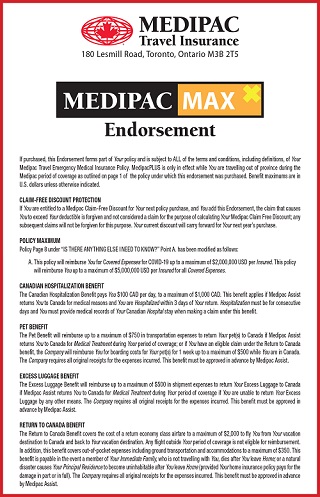
MedipacMAX Travel Insurance Endorsement
- Increased Policy Benefit Maximum to $5 million USD – including COVID-19
- Protect your Discounts in the event of a claim
- $10,000 Accidental Death Insurance
- $5,000 Relocation Benefit
- $1,000 Pet Benefit
- $1,000 Excess Luggage Benefit
- $3,000 Return To Canada Benefit
- $2,000 Canadian Hospitalization Benefit
- $5,000 Inpatient Rehabilitation benefit
Download
Travel Insurance Plan
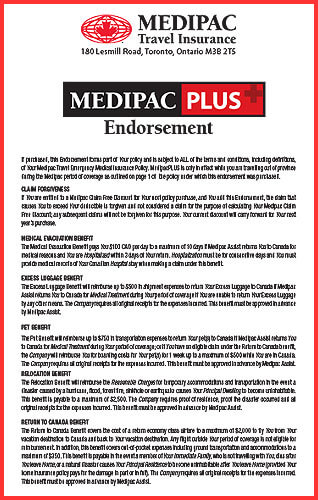
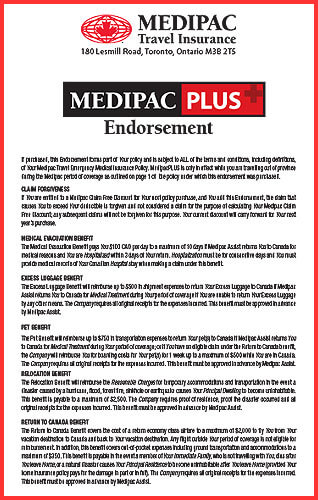
MedipacPLUS Travel Insurance Endorsement
- $500 Pet Benefit
- $500 Excess Luggage Benefit
- $2,500 Relocation Benefit
- $2,000 Return To Canada Benefit
- $1,000 Canadian Hospitalization Benefit
- $5,000 Accidental Death Insurance
- $2,500 Inpatient rehabilitation benefit
- Protect your Claim-Free Discount in the event of a claim
- Increased Policy Benefit Maximum to $5,000,000 USD
o NOTE: COVID-19 coverage limited to $2 million USD
o For $5 million COVID-19 coverage you MUST upgrade to MedipacMAX.
Download
Travel Insurance Plan
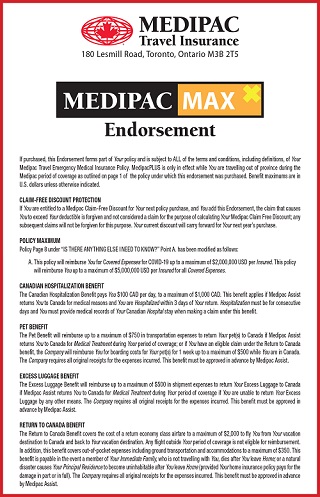
MedipacMAX Travel Insurance Endorsement
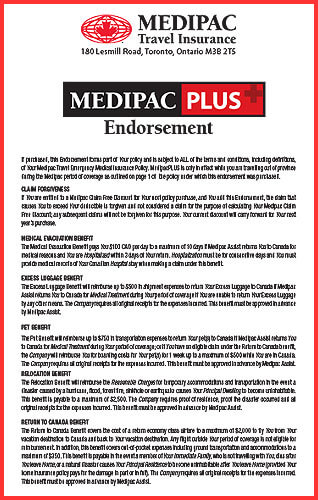
MedipacPLUS Travel Insurance Endorsement